Prescription Drug Affordability Boards
States across the country are experimenting with Prescription Drug Affordability Boards (PDABs) to address the price of medicine. Each state has a different approach. Several exist to negotiate supplemental Medicaid rebates; others make recommendations to limit costs.
A third group of PDABs is particularly concerning because they have the power to set state-wide upper payment limits (UPLs) that cap both the amount pharmacy or provider can pay to buy a medicine and the amount they can be reimbursed for it.
This strategy presents a big problem for pharmacies and providers. UPLs set a ceiling on the amount a pharmacy can pay and be reimbursed for a drug, but they don't control the price at which a medicine is sold. Learn why PSM opposes Upper Payment Limits.
PSM resources about PDABs
Click the state to for links to PDAB program pages, links to meeting notes, etc.
States with PDABs
States in dark red have passed legislation to create a PDAB.
Bright red states have PDABs that can set Upper Payment Limits. Yellow states are states with proposed PDAB legislation. States in Blue has repealed their PDABs.
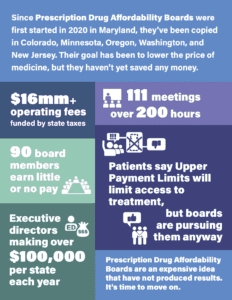
Five years of PDABs by the numbers
PDABs have been adopted in Colorado, Maryland, Minnesota, Oregon, Washington, and New Jersey since 2020. Their goal has been to lower the price of medicine, but so far they haven't saved any money. Download the.pdf.
Five years of PDABs: Broken promises, rising costs, and risks to access
Learn more about how PDABs have failed to fulfill their promise for the last five years, and what they should be focusing on to lower drug costs.
PSM Podcasts & Videos
Video: Will Colorado create a black market in medicine with price controls? (June 1, 2024)
Podcast: Shabbir Imber Safdar and Krystalyn Weaver (NASPA) discuss PDABs (May 29, 2024)
Podcast: Shabbir Imber Safdar and Jen Laws (CANN) discuss PDABs (March 20, 2024)
Other resources
Money-saving Medicaid reforms - NCPA handout
Instead of Upper Payment Limits, state legislatures looking to save money should learn from states that have implemented Medicaid reforms that have saved hundreds of millions of dollars. Documented in this handout from the National Community Pharmacists Association, it shows multiple legislative reforms and the savings they created for the state while also enhancing patient coverage and strengthening pharmacy, a key element of a state's health care resiliency.
Avalere study 2024
Study assessed how health plans may view Upper Payment Limits, including implementation considerations and impacts on providers and patients (e.g., plan benefit design). Six double-blinded interviews with health insurance executives revealed that a UPL is unlikely to create savings for the patients, and may affect formulary placement in favor of medicine with better rebates.
Prescription Drug Affordability Board State Legislation
PDABs by State
Colorado
In 2021, Colorado established a prescription drug affordability review board (PDAB) to reviews and recommends ways to address costs, including setting upper payment limit for certain prescription drugs.
Over the course of 2023 and 2024, Colorado’s PDAB selected five drugs—Cosentyx, Enbrel, Genvoya, Stelara, and Trikafta—and declared Cosentyx, Enbrel, and Stelara unaffordable. Enbrel drugmaker Amgen filed a legal challenge that delayed the boards' price setting, but that case was dismissed in March 2025, clearing the way for the board to move forward with price setting.
Website: Colorado Prescription Drug Affordability Review Board & Advisory Council
Pertinent legislation: SB 21-175/Chapter 240 (June 2021); CO HB 23-1255 (May 2023)
Reports:
Meeting summaries
PDAB meetings:
PDAAC meetings:
Other materials:
Maine
The board determines annual spending targets for prescription drugs purchased by Maine public payers and makes recommendations to achieve the targets.
Records: Through June 2024 | July 2024 —
Pertinent legislation: LD 1499/Chapter 471 (June 2019); LD 120 (2021) (July 2021)
Reports
- 2021 Report (March 2022)
- 2022 Report (January 2023)
- 2023 Report (not dated)
- 2024 Report (not dated)
Maryland
The board studies Maryland's pharmaceutical distribution and payment system and policy in other states and countries to lower the list price of pharmaceuticals. This includes setting upper payment limits, using reverse auction marketplaces, and implementing a bulk purchasing process.
Website: Prescription Drug Affordability Board Website
Pertinent legislation: HB 768/Chapter 692 (May 2019); HB 1100/Chapter 425 (May 2020); HB 279/SB 2022 (April 2023); HB 200/SB 181 (April 2023)
Reports
- Study of the Operation of the Generics Drug Market (June 2022)
- 2022 Annual Cost Review Report (December 2022)
- 2023 Annual Cost Review Report (December 2023)
- Upper Payment Limit Action Plan (September 2024)
- Supply Chain Report (September 2024)
- 2024 Annual Cost Review Report (December 2024)
Meeting summaries
PDAB meetings:
PDASC meetings:
Massachusetts
The state's Health Policy Commission negotiates Medicare supplemental rebates with drug manufacturers.
Website: Drug Pricing Review
Pertinent statutes:
- Medicaid Model Enhanced Negotiating Authority (HB 4000 - Section 46, FY 2020 Budget)
- General Law - Part I, Title II, Chapter 6D, Section 8A
Minnesota
The board reviews the affordability of certain drugs and may establish upper payment limits with reference to the federally negotiated Medicare maximum fair price, if one exists.
Website: Prescription Drug Affordability Board
Pertinent statutes: SF 2744 (May 2023)
New Hampshire
The board determines spending targets for specific drugs and recommends policies to meet those targets.
Website: Prescription Drug Affordability Board
Pertinent statutes: HB 1280/Chapter 13 (enacted July 2020)
Reports:
New Jersey
The council will formulate policy recommendations that will to protect residents, state and local governments, health benefits plans, health care providers, licensed pharmacies, and other stakeholders within the state health care system from the high costs of prescription drug products.
Website: Drug Affordability Council
Pertinent statutes: P.L. 2023, Chapter 106 (July 2023)
New York
The state's Drug Utilization Review Board negotiates Medicare supplemental rebates with drug manufacturers.
Website: Medicaid Drug Utilization Review Board
Pertinent statute: SB 2017-S2007
Annual reports:
Ohio
The council was established to recommend the best ways to achieve prescription drug price transparency; create the most affordable environment for purchasing prescription drugs; leverage the state's purchasing power; and create efficiencies across different health care systems.
Website: Prescription Drug Transparency and Affordability Council (cached copy from April 2021)
Pertinent statute: Section 125.95 | Prescription drug transparency and affordability advisory council (October 2019)
Report: 2020 Report of Recommendations
Oregon
The board conducts affordability reviews on prescription drugs and insulin products. It identifies nine drugs and at least one insulin product that may create affordability challenges for health care systems or high out-of-pocket costs for Oregonians each year. The board is developing a plan for establishing upper payment limits on drugs subject to affordability reviews. The board provides also makes policy recommendations, reports and letters for the Oregon Legislature.
Website: Oregon Prescription Drug Affordability Board | Affordability Reviews
Pertinent statutes: SB 844/Chapter 598 (July 2021); SB 192 (August 2023)
Reports:
- 2022 Report for the Oregon Legislature (December 2022)
- Final Rule: Selecting Prescription Drugs for Affordability Review (July 2023)
- 2023 Generic Drug Report for the Oregon Legislature (June 2023)
- 2023 Report for the Oregon Legislature (December 2023)
- 2024 Generic Drug Report
Meeting summaries
Washington
The board conducts affordability reviews on eligible drugs and may set upper payment limits on drugs it determines are unaffordable for consumers.
Website: Washington Prescription Drug Affordability Board
Pertinent statute: Washington SB 5532 (March 2022)
Reports:
- Annual Report 2023 (December 2023)
- Annual Report 2024 (December 2024)
Meeting summaries
PDAB meetings:
- July 16, 2024
- November 13, 2024
- January 15, 2025
- May 21, 2025
- July 15, 2025
- November 19, 2025
PDAB Advisory Group meetings: